Or also: open spine, spina bifida aperta, myelomeningocele, myelocele, rhachischisis
Causes and effects
What is commonly referred to as “open spine” is the most common cause of congenital physical disability and is diagnosed in approximately one in 3,000 children after birth. The malformation usually occurs at the level of the lumbar spine and sacrum and is caused by a failure of the spinal cord and vertebral arches to close at a very early stage of pregnancy.
“Open spine” can therefore be detected early on by ultrasound. The first signs of the condition are usually seen in prenatal ultrasound scans, which show that the baby’s head is too small in width and circumference, the brain ventricles are enlarged, and there are characteristic sonographic signs (lemon sign, banana sign, intracranial translucency).
A comprehensive overview of the spectrum of this often serious malformation can be found here: Neonatology Scan 2024

Depending on which part of the spine (sacrum, lumbar region, thoracic region, or cervical region) is surrounded by amniotic fluid, which can cause additional damage, spina bifida can result in varying degrees of paralysis, sensory disturbances, and, in some cases, impairments such as incontinence.
DAMAGE BASED ON THE LEVEL OF MALFORMATION
For example, if the malformation occurs from the second lumbar vertebra (L2) upwards, affected, untreated children are rarely able to walk independently later in life.
At the same time, the chances of being able to walk increase significantly with lower malformations (L4/5), even without prenatal surgery. However, aids such as orthoses or crutches are often still required for walking. According to a literature review by Joseph Bruner and Noel Tulipan, pioneers in fetal surgery for spina bifida, 60 percent of all patients retain the ability to walk, even without prenatal therapy, if the damage to the back is located in the area of the fourth lumbar vertebra.
In 90 percent of children, the chances of walking are good if the damage is located in the area of the fifth lumbar vertebra. However, aids such as orthoses are often still necessary in these cases. If, on the other hand, the spina bifida is located at the level of the sacrum, almost all affected children are able to walk later in life.
An additional feature of spina bifida is the displacement of parts of the cerebellum and brain stem (Chiari type II malformation; Arnold-Chiari malformation) into the spinal canal of the cervical spine, which is usually present. This abnormality is found in almost all affected individuals and promotes the accumulation of cerebrospinal fluid, which in turn leads to enlargement of the cerebral ventricles. The result is hydrocephalus, commonly known as “water on the brain.”
Important to know: This disorder in brain development is not synonymous with mental disability! On the contrary, most children with “open back” have normal intelligence. We emphasize this because unfounded fears in this matter often lead to abortions. If you receive such a diagnosis for your unborn child, we therefore strongly advise you to seek further advice from experienced spina bifida specialists.
GENERAL DISABILITIES ASSOCIATED WITH SPINA BIFIDA
However, dysfunction of the bladder and rectal muscles, including the innervation of their sphincters, must be expected in almost every child who has not undergone surgery before birth. Thanks to numerous aids, these disorders no longer prevent a largely normal social life.
An additional feature of spina bifida is the simultaneous displacement of parts of the cerebellum and brain stem (Chiari type II malformation; Arnold-Chiari malformation) through the skull base (foramen magnum) into the spinal canal of the cervical spine. This abnormality is found in almost all affected individuals and promotes the accumulation of cerebrospinal fluid, which in turn leads to enlargement of the ventricles. The result is hydrocephalus, commonly known as “water on the brain.”
Important to know: Chiari type II malformation and mild hydrocephalus are not synonymous with mental disability! On the contrary, most children with “open back” – in the absence of genetic abnormalities detected in amniotic fluid testing – can expect normal intellectual development. We emphasize this fact so clearly because unfounded fears in this matter often lead to abortions. If you receive such a diagnosis for your unborn child, we therefore strongly advise you to seek further advice from experienced spina bifida specialists.
Also important to know: Numerous scientific studies have shown that in most unborn babies with spina bifida, paralysis and foot deformities, as well as hydrocephalus, only develop more and more during the course of pregnancy. All prenatal operations on unborn babies with open spine therefore aim to shorten this natural process by several months in order to reduce the extent of damage.
POST-BIRTH CLOSURE OF THE “OPEN BACK”
The closure of the open back performed by pediatric neurosurgeons after birth aims to close the freely protruding spinal cord structures for cosmetic reasons, prevent further loss of cerebrospinal fluid, and prevent infections. An improvement in paralysis, sensory disturbances, and incontinence is expressly not to be expected after postnatal surgery for “open back.”
The accompanying hydrocephalus is often treated during the same procedure by implanting a tube system equipped with a valve (ventriculoperitoneal shunt/VP shunt).
Studies have shown that these symptoms, like others, develop more and more during pregnancy and do not improve after the “open back” is closed after birth. All prenatal surgery on unborn babies with open back, on the other hand, aims to stop this natural process and thus reduce the extent of damage.
Minimally invasive prenatal treatment of spina bifida at the DZFT
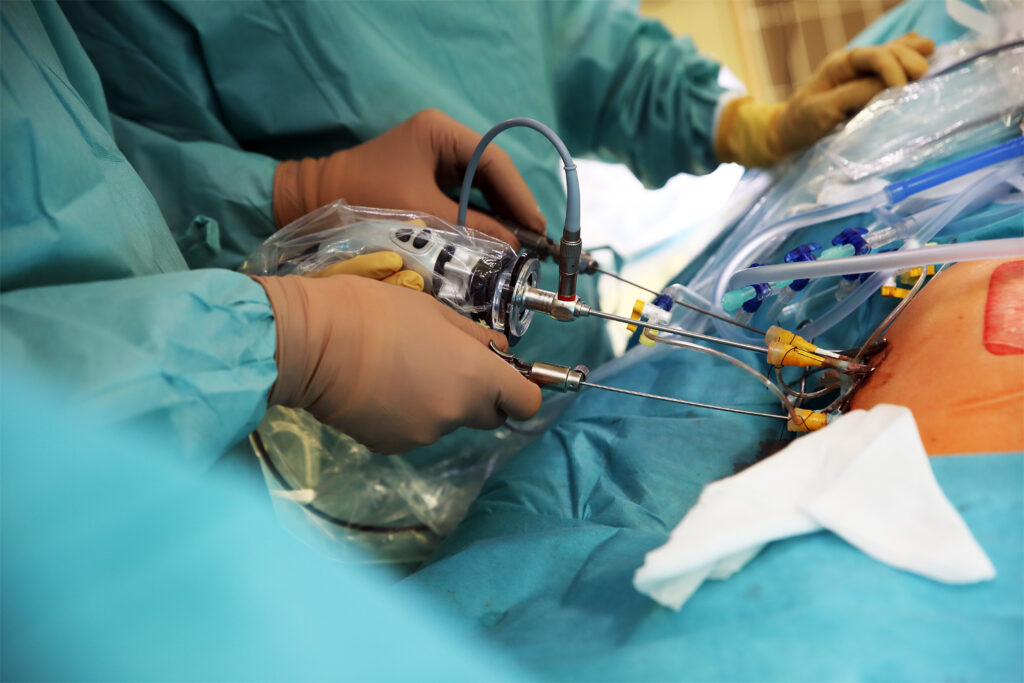
In order to significantly improve leg function and continence in unborn babies affected by spina bifida, mitigate accompanying brain changes, and reduce the need for a VP shunt, the head of the DZFT, Professor Thomas Kohl, MD, developed a completely percutaneous, minimally invasive prenatal keyhole surgical method This was the first method in the world to be performed without opening the mother’s abdomen.
We use this method to close the “open back” usually between the 25th and 29th week of pregnancy. This reduces the negative effects in the uterus by several months, with great benefits for most of our little patients. Today, more than 20 years after the first operation, the DZFT has performed nearly 300 procedures, giving it the longest and most extensive experience of any single center in the world in the minimally invasive prenatal treatment of unborn babies with open spine.
Background
For decades, numerous scientific studies have shown that the severity of spina bifida symptoms is not determined solely by the malformation of the spine and nerve tissue in the earliest stages of a baby’s development.
Repeated ultrasound examinations throughout pregnancy, as well as experimental and tissue studies, have increasingly shown that in most unborn babies with spina bifida, paralysis, foot deformities, and hydrocephalus develop more and more as pregnancy progresses.
To prevent this gradual loss of function, we close the “open back” as early as the middle of the 20th week of pregnancy. This reduces the negative influences in the uterus by almost four months, with great benefits for most of our little patients.
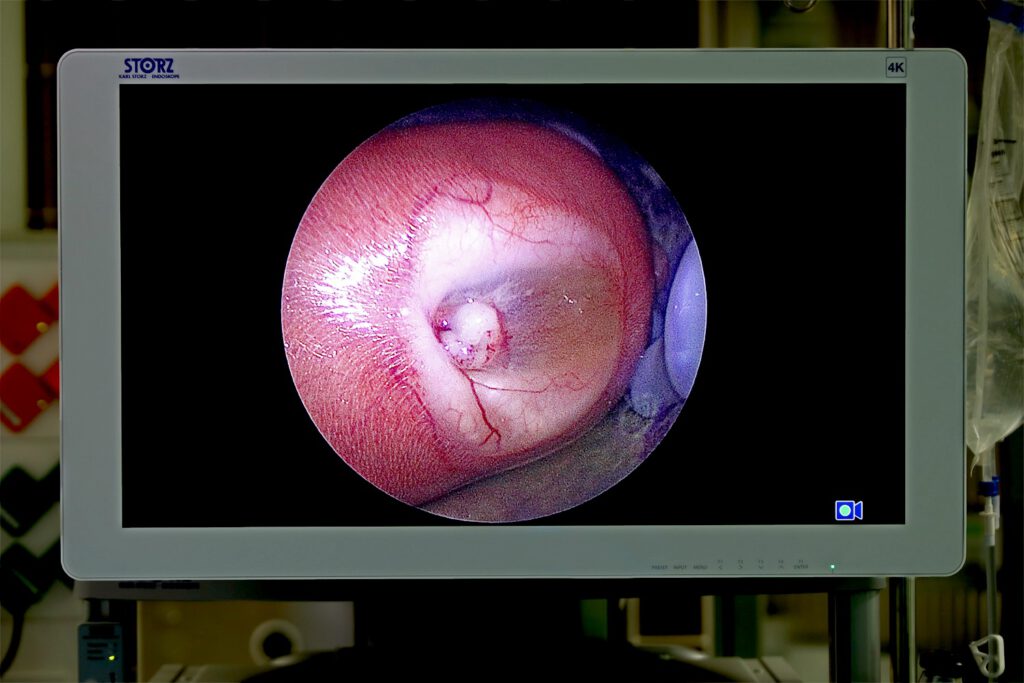
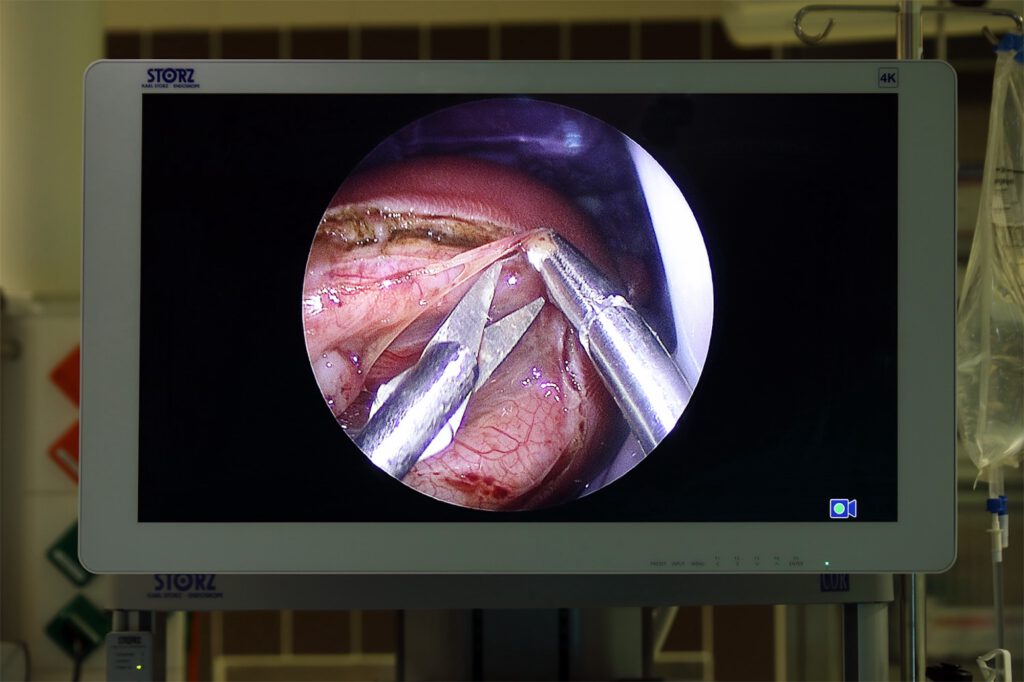
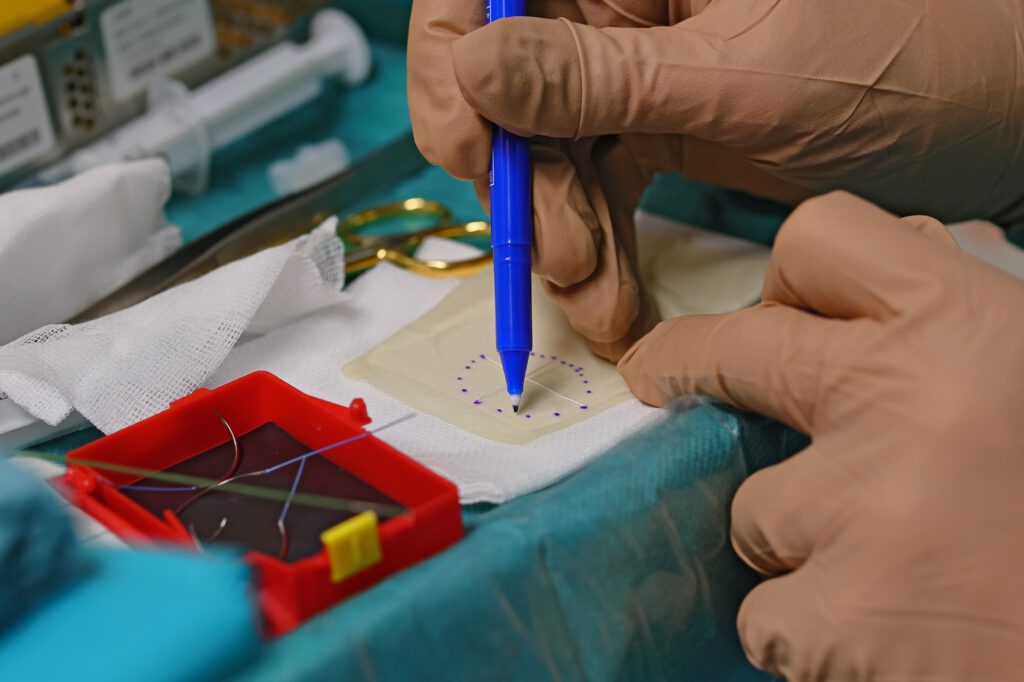
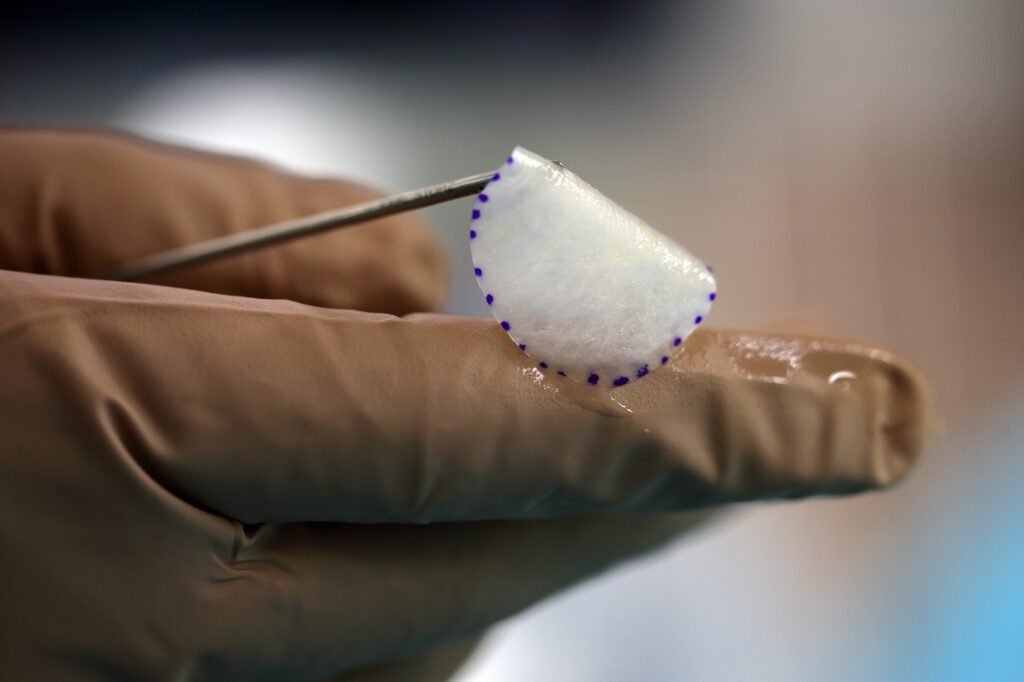
At the DZFT, we avoid large incisions and thus the opening of the abdomen and uterus during pregnancy (open fetal surgery, see below) whenever possible by using our minimally invasive fetoscopic procedure, which can be performed without incisions in the mother’s abdomen. Instead, the open area on the back of the unborn baby is closed with three small surgical tubes, each with an outer diameter of only five millimeters.

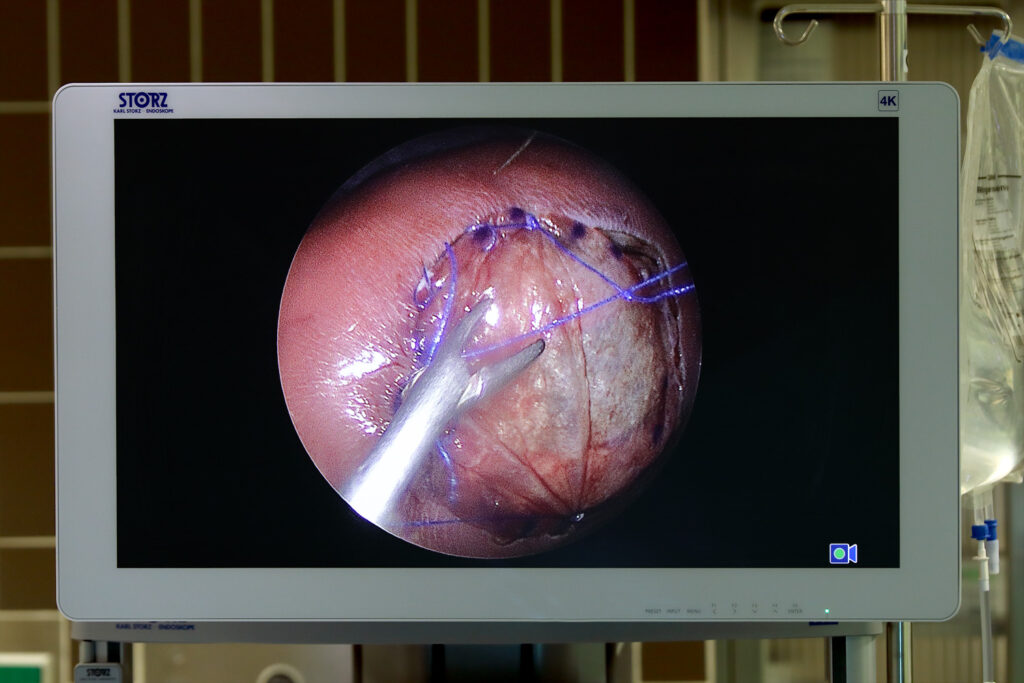
This means that the mother’s abdominal wall and uterus remain virtually intact and heal very quickly. Thinning or tearing of the uterine wall is not observed with our minimally invasive method.
This is an enormous advantage over “open fetal surgery,” which involves surgical opening of the mother’s abdomen and uterus. The open procedure is not only very stressful for pregnant women. In about one-third of cases, uterine wall weaknesses are observed, which make normal delivery too risky and also pose a considerable risk for subsequent pregnancies. In the worst case, after open fetal surgery, the pregnant woman is at risk of a complete rupture of the uterine wall during the pregnancy of the operated child or in subsequent pregnancies, with the risk of severe bleeding. In addition, the deep anesthesia required for the invasive procedure has an adverse effect on the child’s circulation, which explains the more frequent occurrence of cerebral infarcts after open fetal surgery.
These serious complications do not occur with minimally invasive surgical methods.
Furthermore, we only recommend open surgery in absolutely exceptional cases: The results of minimally invasive prenatal treatment of spina bifida are at least as good, if not better, than those of open surgical methods (literature reference).
Based on all this experience with our surgical method, we have deliberately decided against multi-layer closure of the malformation, as is often offered in open fetal surgery and, more recently, by some groups performing fetoscopic surgery. With minimally invasive single-layer closure, the spinal cord is treated much more gently than with attempted multi-layer coverage – a clear advantage for preserving the child’s leg function.

Further advantages of our surgical method are summarized here:
– Almost all children born after completely percutaneous surgery and hybrid surgery are born in the last trimester of pregnancy: The average age at delivery after completely percutaneous surgery is 33–34 weeks of gestation, and 36 weeks of gestation after hybrid surgery. However, this does not represent a clear advantage for the hybrid procedure for the children treated, as serious complications of premature birth are rare after the 30th week of pregnancy.
– In the majority of cases, our prenatal surgery can reverse the cerebellar displacement that contributes to hydrocephalus.
– The mobility of the legs at the time of the procedure can be maintained after single-layer closure; the results are therefore remarkably positive compared to most children who did not undergo prenatal surgery.
Many of “our” children with high lesions from the 11th thoracic vertebra (Th11) to the 2nd lumbar vertebra (L2), who would in all likelihood have been confined to a wheelchair without prenatal surgery, learned to walk after minimally invasive prenatal surgery.
– In 90% of children, the minimally invasive single-layer prenatal closure also replaces the surgical closure of the open back after delivery.
– If narrow brain ventricles are still present in the unborn patients we treat at the time of the procedure, they require implantation of a brain fluid drainage system (shunts) much less frequently after birth. Compared to children who undergo surgery after birth, this reduces the need for hydrocephalus surgery (VP shunt placement) by about half.
Meanwhile, supported by the work at the DZFT, minimally invasive fetal surgery for unborn babies with spina bifida is gaining ground worldwide and replacing open surgery.
The recommended time for minimally invasive closure of the open back at the DZFT is at the beginning of the period between the 25th and 27th week of pregnancy.
Based on our experience, this period offers the best surgical conditions for preventing functional loss of your child’s legs, rectum, and sometimes also the bladder, as well as for improving the accompanying brain changes. As a pregnant woman, you will be admitted to our hospital two days before the procedure and discharged home about a week later. We ask that you take it easy physically for the rest of your pregnancy.

More than half of the 24 fetuses (July 2018–July 2024) we have operated on over the past 12 years with particularly high lesions from the 11th thoracic vertebra to the 2nd lumbar vertebra learned to walk after our particularly spinal cord-sparing, minimally invasive prenatal surgery. Without fetal surgery, children affected in this way hardly ever learn to walk. However, even after open fetal surgery at a major European center, a recent publication reported a 0% walking rate for this level of malformation (Brun B, et al. Motor function outcomes in children with open prenatal repair of Spina Bifida Aperta at 36-month follow-up: The Zurich cohort. Pediatr Rehabil Med 2023;16(4):595-604. doi: 10.3233/PRM-220096).
However, there are clear limits to minimally invasive procedures!
Paralysis that has already occurred before the procedure cannot be reversed, nor can advanced hydrocephalus.
The operation also has no effect on severe, very deep displacement of the cerebellum and brain stem.
In our experience, there is also a small risk of about 3% that an unborn child will die as a result of an infection caused by the procedure or premature birth. Taking all these factors into account, we thoroughly weigh up the benefits and risks of prenatal surgery for each pregnant woman and each child.
In addition, depending on the decision made by the expectant mother, further treatment options are available at our clinic in collaboration with the departments of neonatology, pediatric neurosurgery, and prenatal medicine.
If you have any further questions about minimally invasive treatment for spina bifida or would like to make an appointment, please contact us daily between 10 a.m. and 5 p.m. on 0175/597-1213 or send us an email. If you have already decided to have the procedure performed at another clinic, we will be happy to advise you and offer a prognostic second opinion on your child’s condition.
If you only reach our answering machine, please leave your name and a telephone number where we can call you back.
Regardless of your decision for or against prenatal surgery, Dr. Philip Kunkel, Head of the Pediatric Neurosurgery Department, and Prof. Raimund Stein, Head of the Pediatric, Adolescent, and Reconstructive Urology Department at the University Medical Center Mannheim (UMM).
You can also obtain a wealth of important information about spina bifida from the nationwide self-help group BfVEK. They or we can also put you in direct contact with many of our former prenatal surgery patients and their families. This will allow you to obtain first-hand information.
If you have any questions about our scientific work, publications, or further results of our minimally invasive fetoscopic surgical method for unborn babies with spina bifida, please feel free to contact us by email or phone (see above) and use the medical database: Pubmed
Please note: The content of our website is for informational purposes only and is not intended to replace personal advice from us or other recognized medical professionals in this field. For all individual questions and decisions regarding your health and that of your child, we strongly recommend that you and your family members contact us, your doctor, and/or other experts in person.
