In identical twin pregnancies, abnormal vascular connections (anastomoses) can occur on the placenta, causing a dangerous transfer of blood from one fetus—the donor—to the other—the recipient. This condition is known as “feto-fetal transfusion syndrome” or “twin-to-twin transfusion syndrome.”
In severe cases, this leads to pronounced growth problems in the donor and circulatory problems in both children. If twin-to-twin transfusion syndrome is left untreated, the circulatory problems alone pose a risk that both babies will die or become seriously ill before delivery.
Typically, the recipient produces far too much amniotic fluid, causing the pregnant woman to suffer from a painfully tense abdomen, back pain, and shortness of breath. Since the amount of amniotic fluid can increase very suddenly and rapidly, all pregnant women with twin pregnancies who experience the symptoms described above should immediately consult a prenatal care practice or gynecological clinic. This applies even if the twins were previously thought to be fraternal. Delaying treatment at this stage can result in the loss of the pregnancy due to cervical incompetence, premature labor, rupture of the membranes, and premature birth.
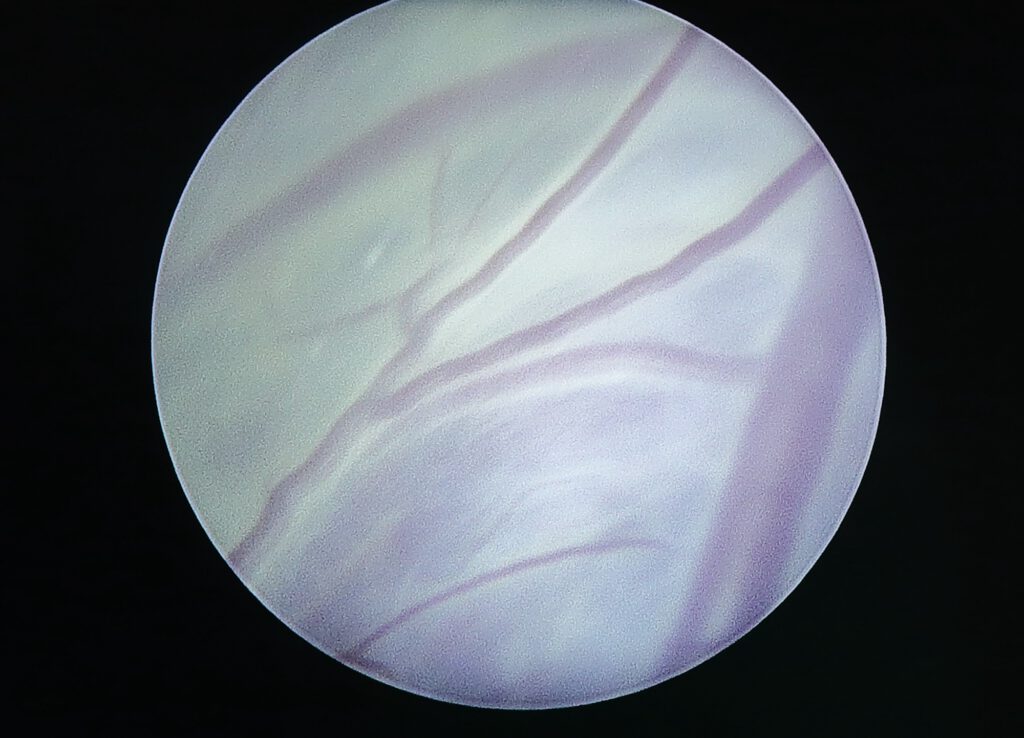
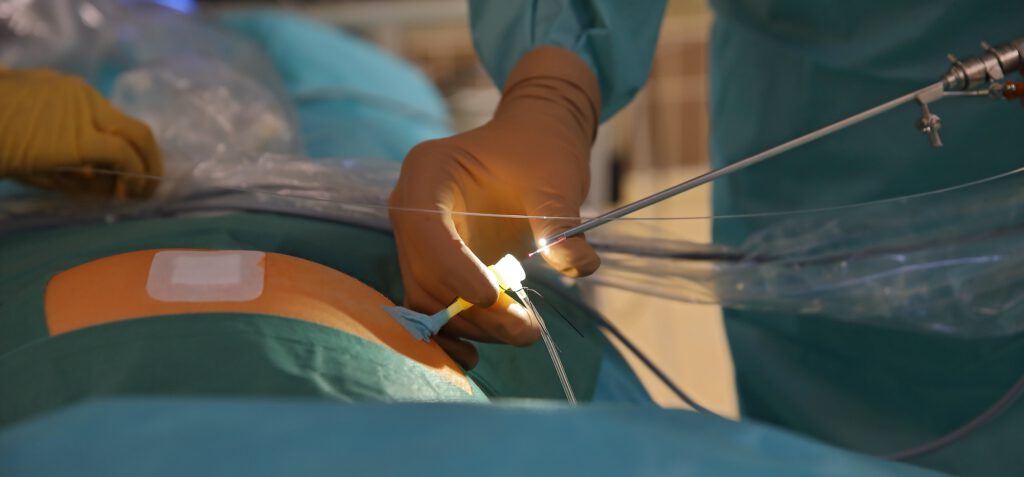
Fortunately, FFTS can be reliably diagnosed and assessed in terms of severity using ultrasound. If the situation becomes life-threatening for one or both babies, or if the pregnancy is endangered by too much amniotic fluid, the placental vessels causing the problem can be closed using laser energy after local anesthesia of the mother’s abdominal wall.

In around 80 percent of cases, at least one of the children survives. In around 60 percent of all cases, both children can be saved in this way. An estimated 80 percent of surviving children are born after the 30th week of pregnancy. At this stage, the risk of damage due to early birth is already low. The surviving children are also usually born healthy. Nevertheless, we would like to point out that there is a small risk (around five percent) of brain damage in these children.
Scientific analyses now recommend minimally invasive fetoscopic closure of the abnormal placental vessels as the best treatment option for this condition. The treatment strategy of “serial amniotic drainage” with the sole aim of repeatedly removing the excess amniotic fluid is now only used in individual cases. This shortens the duration of pregnancy and there is a higher risk of brain damage or death of the children than after fetoscopic closure.
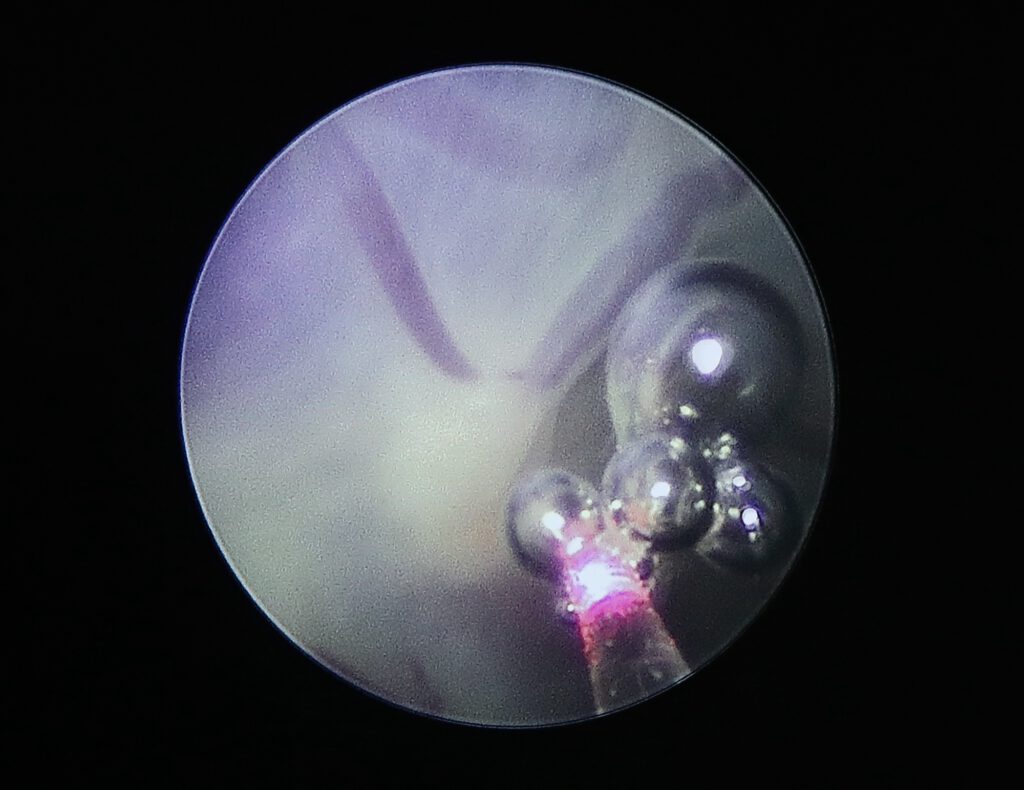
The timing of the procedure is determined by the amount of amniotic fluid and the bladder filling of the unborn child, as well as the extent of the child’s cardiac stress and placental blood flow. We generally perform the procedure at the DZFT between the 16th and 28th week of pregnancy.
As part of the development and improvement of fetoscopic surgical techniques, our center has focused on technically difficult laser procedures. Based on our many years of experience, previous punctures of the amniotic sac (e.g., to reduce the amount of amniotic fluid or due to another previous procedure) do not prevent fetoscopic closure of the abnormal placental vessels. Severe obesity of the expectant mother is also not a criterion for exclusion on our part. If you have been refused a fetoscopic procedure at another center for the above-mentioned or other surgical reasons (e.g., unfavorable position of the placenta), we will be happy to provide you with advice and treatment.
If you have any further questions about the minimally invasive treatment of this prenatal condition, you can reach us daily between 10 a.m. and 5 p.m. at (0175) 597-1213 or send us an email. If you only reach our answering machine, please leave your name and a phone number where we can call you back.
Please note: The content of our website is for informational purposes only and is not intended to replace personal advice from us or other recognized medical professionals in this field. For all individual questions and decisions regarding your health and that of your child, we strongly recommend that you and your family members consult us, your doctor, and/or other experts in person.
