During routine ultrasound examinations during pregnancy, special attention is paid to the baby’s heart. In some cases, it may be discovered that a baby already has a significantly undersized left ventricle in the womb, which will not be able to supply the body with blood after birth. This heart defect is known as hypoplastic left heart syndrome, or HLHS.
For many years now, children affected by this condition have been able to receive help after birth in the form of pediatric cardiology and cardiac surgery. The aim of these measures is to optimize the circulation so that it can be supplied by only one heart chamber instead of two.
In some children, HLHS is caused by early, complete closure of the aortic valve (aortic valve atresia). This is accompanied by a pronounced underdevelopment of the initial section of the large artery, the ascending aorta. If this has a diameter of only 2.5 mm or less, it is considered a risk factor for postnatal treatment.
In addition, many children with HLHS also have a significantly underdeveloped aortic arch, which must be widened after birth using Gore-Tex material. If the aortic arch is very narrow, there is little tissue available for the aortic arch to expand sufficiently as the child grows. This results in reoperations.
If your unborn child with HLHS has a very small, thread-like ascending aorta or if it cannot be visualized at all. Even if the aortic arch is significantly underdeveloped, a significant catch-up growth of the ascending aorta and also of the aortic arch can be achieved with a non-invasive drug treatment method, even shortly before the end of pregnancy.
The completely non-invasive drug treatment method was developed by Prof. Thomas Kohl at the DZFT and used for the first time in the summer of 2007: chronic intermittent materno-fetal hyperoxygenation, or oxygen therapy or Kohl procedure for short.
The principle of oxygen therapy is easy to understand: before birth, the pulmonary vessels of the unborn child are still narrow. This makes sense because the child is not yet breathing independently, but exchanges oxygen and carbon dioxide via the placenta.
Immediately after birth, however, these vessels must dilate significantly so that the oxygen contained in the air can enter the child’s blood via the airways and alveoli. The strongest trigger for this vital dilation of the pulmonary vessels is oxygen itself. We make use of this mechanism in “oxygen therapy” (see literature below).
When a pregnant woman inhales oxygen, a small portion of it passes through the placenta to her unborn child. In many cases, this small portion is sufficient to cause a pronounced dilation of the lung vessels and an increase in pulmonary blood flow in babies with a too small aortic arch.
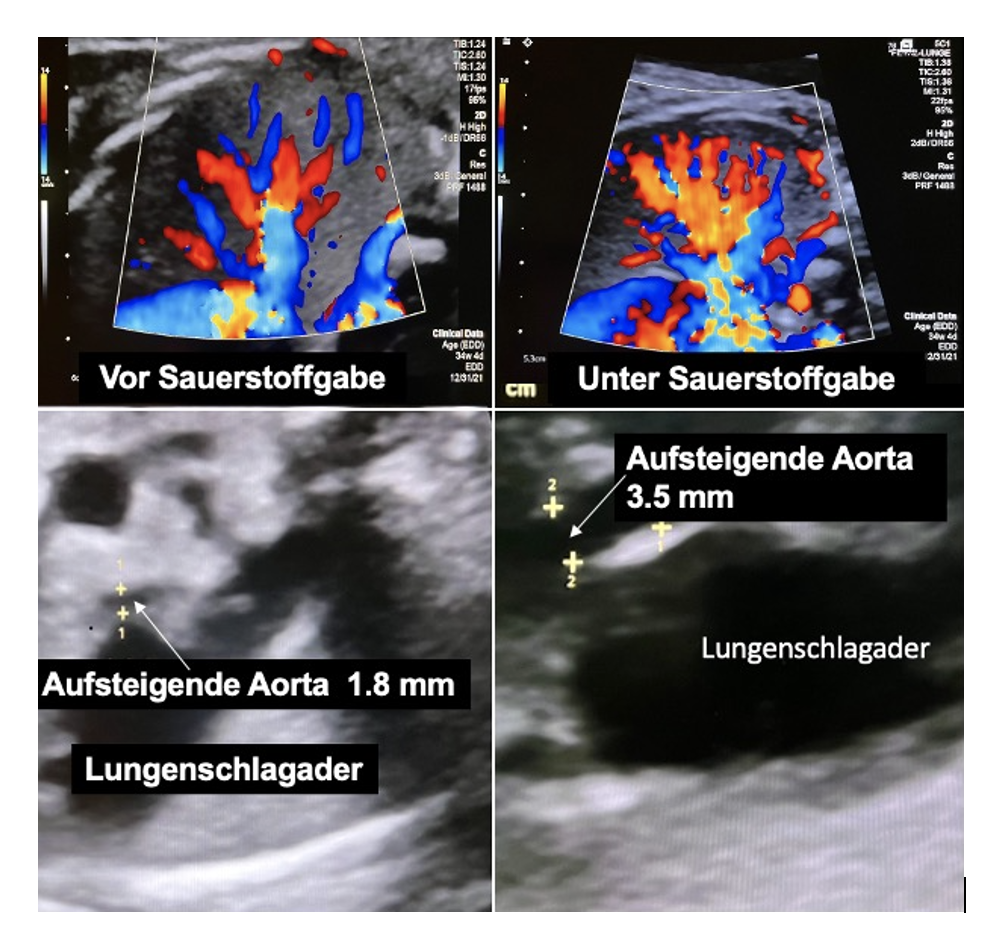
The greatly increased blood flow to the lungs also requires a significant increase in cardiac output. This is accompanied by a marked increase in blood flow in the coronary arteries. Since the aortic valve is closed (atretic), these arteries are supplied retrograde via the ascending aorta.
Due to the increased blood flow, we observed in a small cohort of unborn babies that there was a significant catch-up growth stimulus in this area during the last weeks of pregnancy. This can be observed after only about a week of therapy through improved sonographic imaging of the ascending aorta and the aortic arch. This offers advantages for postnatal surgical treatment of HLHS (Norwood I or Comprehensive Stage II).
To avoid misunderstandings: In HLHS, the left ventricle cannot grow any further, so a single-ventricle circulation will be necessary in all cases! This is an important difference from HLHC, the hypoplastic left heart complex. In this spectrum, the left side of the heart still functions, but is too small and can be positively influenced by oxygen therapy during growth.
For further information and advice on prenatal and postnatal treatment options for HLHS, we are available daily between 10 a.m. and 5 p.m. on (0175) 597-1213 or by email. You are also welcome to leave us your name and a telephone number where we can call you back.
Note: The content of our website is for informational purposes only and is not intended to replace personal consultation with us or other recognized medical specialists in this field. For all individual questions and decisions regarding your health and that of your child, we strongly recommend that you and your family members consult us, your doctor, and/or other experts in person.
Literature
1. Chronic intermittent materno-fetal hyperoxygenation in late gestation may improve on hypoplastic cardiovascular structures associated with cardiac malformations in human fetuses. Kohl T. Pediatr Cardiol. 2010 Feb;31(2):250-63. doi: 10.1007/s00246-009-9600-5. Epub 2009 Dec 19. PMID: 20024652
2. Chronic intermittent maternofetal hyperoxygenation (Kohl procedure) for the treatment of flow-related cardiovascular hypoplasia in human fetuses. Kohl T. Ultrasound Obstet Gynecol. 2015 Dec;46(6):746. doi: 10.1002/uog.15747.
3. Kohl T. Lifesaving Treatments for the Tiniest Patients—A Narrative Description of Old and New Minimally Invasive Approaches in the Arena of Fetal Surgery Children 2023, 10(1), 67;
https://doi.org/10.3390/children10010067
4. Zeng S et al. Sustained maternal hyperoxygenation improves aortic arch dimensions in fetuses with coarctation. Sci Rep 6, 39304; doi: 10.1038/srep39304 (2016)
