Prenatal examinations can detect or rule out numerous diseases and malformations in a child while it is still in its mother’s womb. Approximately one in 2,500 children has a hole in the diaphragm, known as a diaphragmatic hernia. Half of these children are otherwise completely normal and show no other malformations.
Nevertheless, such a hernia can have fatal consequences for affected children. Due to the lack of closure of the diaphragm, the abdominal and chest cavities are not separated from each other, allowing the abdominal organs (such as the stomach, spleen, liver, and intestines) to move into the child’s chest cavity. This causes the baby’s lungs to be compressed in the womb and severely impedes their development. If the baby is born in this condition, they are often critically underdeveloped due to the lack of space.
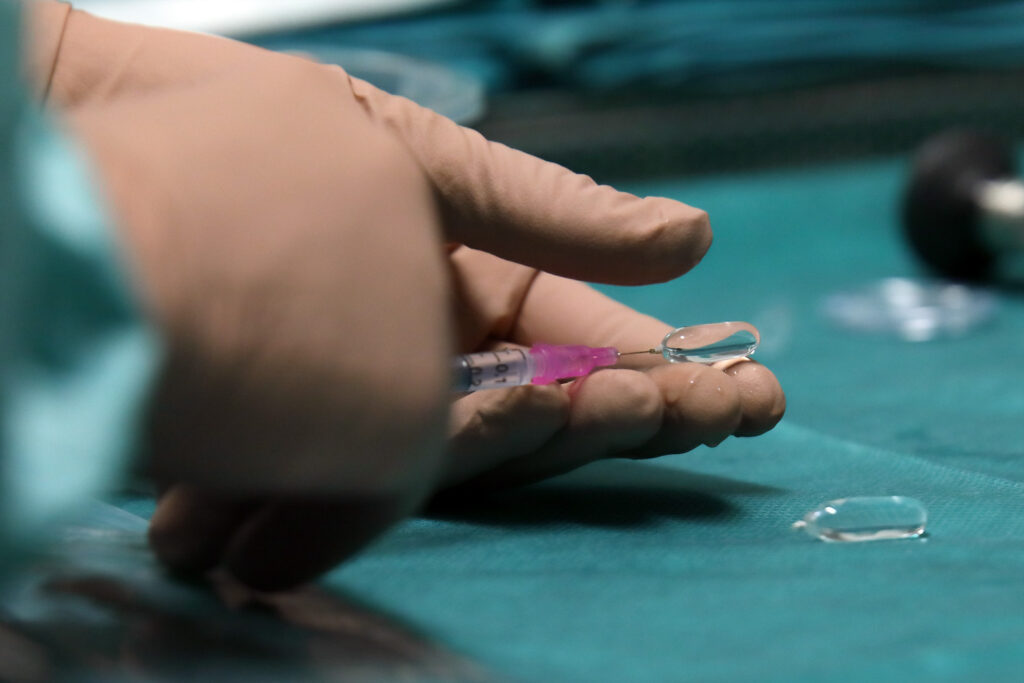
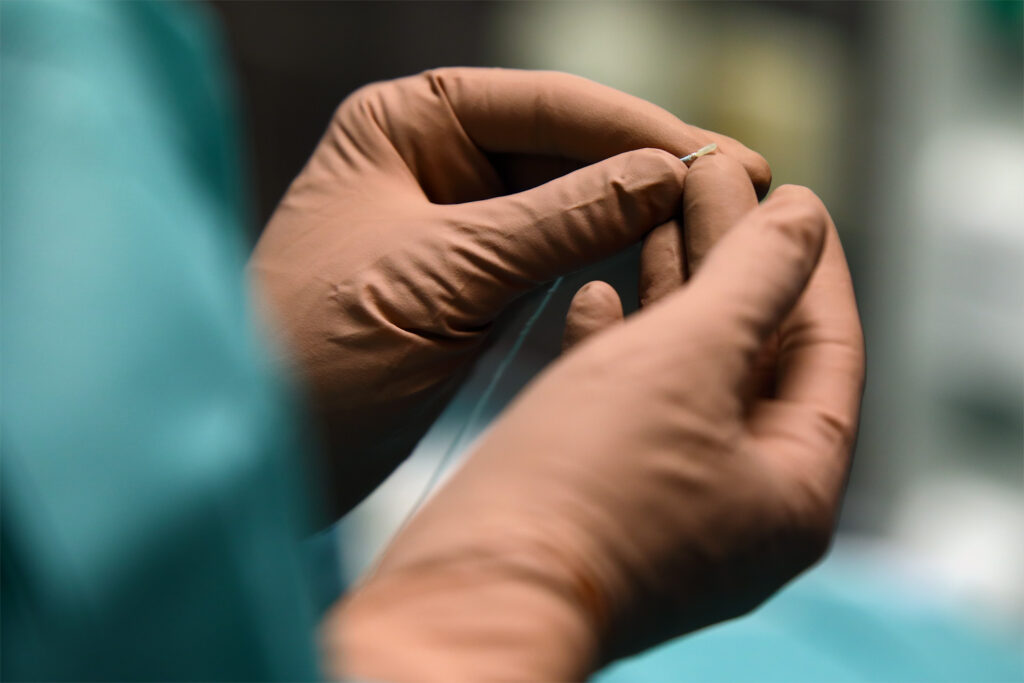
To increase the chances of survival for unborn babies with even the smallest lungs, we perform a minimally invasive prenatal procedure at the DZFT: By temporarily closing the baby’s windpipe (fetoscopic tracheal balloon occlusion) for a period of about two to four weeks, fluid that is normally produced by the lungs is prevented from flowing into the amniotic fluid. As a result, the lungs expand, grow, and become larger. The procedure often improves lung perfusion as well. Prof. Thomas Kohl, head of the DZFT, is one of the pioneers in the surgical development of this method. He introduced it in Germany in 2003.
In our own patient group, around 80 percent of children with severe right-sided diaphragmatic hernias and 70 percent of children with left-sided diaphragmatic hernias survive. We achieve these encouraging results in close cooperation with a center at the Mannheim Children’s Hospital that specializes in the postnatal treatment of newborns with diaphragmatic hernias. Without prenatal treatment, the estimated survival rate for both types of the disease is only around 30 percent.
The prenatal procedure is performed at the DZFT under short anesthesia that is safe for both mother and child, preferably from the 33rd week of pregnancy, in order to give your child the best possible start in life in every respect. This strategy of performing tracheal closure at a late stage of pregnancy was developed by the head of the DZFT, Prof. Thomas Kohl, together with his Mannheim colleague Dr. Thomas Schaible, and has proven itself over many years: At this stage, the unborn babies are large enough and sufficiently developed that all available intensive care measures – including temporary artificial lung therapy (ECMO) – can be provided after birth. Serious complications, which are otherwise a typical consequence of premature birth, are also very rare at this stage of pregnancy – another argument in favor of this approach for us.
Unlike the minimally invasive procedure itself, we carry out the diagnostic examinations earlier: from around the 27th week of pregnancy, ultrasound can give a relatively good indication of the severity of your child’s malformation. From the 31st week of pregnancy, special sonographic examinations and magnetic resonance imaging help us to estimate the size and expected function of the baby’s lungs after birth even more accurately. At this point, our treatment strategy will determine whether prenatal surgery is advisable and should be offered to you to improve your child’s prognosis. Of course, you can also contact us at any time during your pregnancy for detailed information and advice about your child’s condition.
And our urgent request to you: If you are an expectant mother and notice that your abdomen feels uncomfortably tight between the 25th and 33rd week of pregnancy, you should immediately go to a clinic that specializes in prenatal procedures! This is almost always caused by a significant increase in the amount of amniotic fluid (polyhydramnios), which can trigger premature labor, shortening of the cervix, rupture of the membranes, and even premature birth. The reason for the increased amount of amniotic fluid is probably the stomach falling into your child’s chest. This can cause the esophagus to bend, preventing the unborn child from absorbing amniotic fluid through their gastrointestinal tract and returning it to the maternal circulation outside the uterus via the placenta.
If the suspicion is confirmed, the excess amniotic fluid must be removed immediately. In such a special case, if the lungs are very small, the amniotic fluid should be removed and the fetal trachea closed fetoscopically as soon as possible – so do not hesitate to contact the DZFT or another clinic specializing in such prenatal procedures if you suspect this condition.
In addition, it is vital for almost all newborns with diaphragmatic hernia who have undergone prenatal surgery to be treated with ECMO within the first few hours of life. “ECMO” stands for “extracorporeal membrane oxygenation” and is a form of intensive care treatment in which a machine partially or completely supports the respiratory function of the small patients, sometimes for several weeks. For ECMO therapy in children with diaphragmatic hernia, the internationally recognized American Extracorporeal Life Support Organization (ELSO) recommends only centers that have experience in this field, i.e., that have performed at least ten ECMO procedures on children with lung disease per year.


Find out more. Regardless of whether you choose to have your “problem child” treated prenatally at our facility or at another institution, the treatment plan should stipulate that the child is only to be delivered at or transferred to a clinic whose medical and nursing staff have sufficient experience with ECMO treatment. For this reason, children treated prenatally at the DZFT are almost exclusively delivered at the University Medical Center Mannheim (or, in exceptional cases where they are born elsewhere, transferred there after birth). At the ECMO center there, approximately 50 children per year are treated for diaphragmatic hernias, about one-third of them using ECMO therapy.
If you have any further questions about minimally invasive prenatal treatment of fetal diaphragmatic hernia or about the expected postnatal lung function, please contact us Monday through Friday between 10 a.m. and 5 p.m. at 0175/597-1213 or send us an email. If you only reach our answering machine, please leave your name and a phone number where we can call you back.
If you have already decided to have the procedure performed at another clinic, we will be happy to advise you and offer a prognostic second opinion on your child’s condition.
Please note: The content of our website is for informational purposes only and is not intended to replace personal consultations with us or other recognized medical specialists in this field. For all individual questions and decisions regarding your health and that of your child, we strongly recommend that you and your family members contact us, your doctor, and/or other experts in person.
